POTENTIAL
RUSSIAN DESTABILIZATION RESULTING FROM AN MDR-TB EPIDEMIC
Milton Copulos, National
Defense Council Foundation
(Note: Hold mouse over images to view captions)
INTRODUCTION
Throughout recorded history, plagues periodically devastated the world's populations. The "Black Death" - bubonic plague - swept through Europe on three occasions, in the 6th, 14th, and 17th centuries. In the worst outbreak, during the 14th century, it reduced Europe's population by one-third between 1347 and 1352. As dramatic as this figure is, the Black Death was not the world's most deadly epidemic. That questionable distinction falls on the Spanish Flu pandemic of 1918, which took 25 million lives around the world in a single year.
With the advent of antibiotics and inoculation many believe that the danger of pandemics like the Spanish Flu were a thing of the past, at least in the developed world. This view, however, is mistaken. The simple truth is that infectious disease remains the leading cause of death in the developing world. Even in the developed world, taken together, infectious diseases rank fourth. Moreover, in the years ahead, the dangers from infection are likely to increase.
Chronic overuse and misuse of antibiotics have given rise to new and potent strains of bacteria. As a result, new and deadly strains of staphylococcus, pneumonia, and tuberculosis, resistant to all but the most advanced drugs, have appeared. At the same time, modern transportation makes it easy for disease carriers to move between continents. Nowhere is this more evident than in regard to tuberculosis.
In the U.S. more than 40 percent of all new cases of TB occur in immigrants. The Centers for Disease Control and Prevention estimated that in just a few years, such individuals could account for the majority of all new TB cases. Of even greater concern is the fact that at least some of these individuals carry multi-drug resistant tuberculosis or MDR-TB. It is this strain, which carries with it the potential to wreak havoc around the globe. Indeed, the World Health Organization has expressed alarm over the rise in TB rates in 1993. Yet, little action has resulted from the warning even though solutions to the problem do exist. Advanced antibiotics are effective against even MDR-TB. But they are expensive. Without international support their use might be beyond the reach of the nations that need them most. It may be that developed nations do not perceive a threat. If this is the case, they need only look at the impact of past pandemics to see what the future could hold.
THE HISTORIC IMPACT OF PLAGUES
 THE
BLACK DEATH
THE
BLACK DEATH
Recent archeological evidence indicates that bubonic plague outbreaks occurred in Europe as early as the fifth century BCE. Thucydides, the Greek historian described the panic, which struck Athens and Sparta in 430 BCE when plague took nearly a third of the population. Evidence supporting his account of the event was discovered in 1994, when workers excavating a subway station uncovered a mass burial site. As many as 1,000 people may have been buried in the site, which was relatively shallow, indicating a hasty burial. Archeologists examining the site determined that the bodies must all have been buried within a few days and without the artifacts normally associated with burial rites at that time. The scholars studying the site believed that these factors confirmed that the bodies found there were victims of the plague Thucydides described.
 But
it was the outbreak that occurred in the 14th century that demonstrated the
real virulence of bubonic plague.
But
it was the outbreak that occurred in the 14th century that demonstrated the
real virulence of bubonic plague.
In the early 1330's China experienced an outbreak of bubonic plague. At the time, China was a major trading trading nation. In October of 1347, several Italian ships arrived in Sicily, having returned from ports on the Black Sea, a key point of entry for goods from China. Many of the crewmembers on the ships were already dying from the plague. The disease spread like wildfire, engulfing the city and surrounding countryside in days.
As winter set in, the disease seemed to subside. What its victims did not know was that this momentary respite was due to the fact that the fleas carrying the disease became dormant in the winter. With the spring thaw, it returned and by August had spread as far as England. This pattern would repeat itself for five agonizing years.
By the time the Black Death had run its course, it would claim fully one-third of Europe's population, some 25 million people. It would also spark far-reaching changes in European society, including widespread peasant revolts, and a loss of church authority.
THE SPANISH FLU EPIDEMIC OF 1918
 A
much closer parallel of the contemporary threat may be found in the Spanish
Flu pandemic of 1918. In terms of sheer virulence, it far outstripped the Black
Death, claiming at least 25 million victims in just one year. In the United
States alone, one in four Americans were stricken with the disease, and some
600,000 died.
A
much closer parallel of the contemporary threat may be found in the Spanish
Flu pandemic of 1918. In terms of sheer virulence, it far outstripped the Black
Death, claiming at least 25 million victims in just one year. In the United
States alone, one in four Americans were stricken with the disease, and some
600,000 died.
The Spanish Flu first surfaced in the U.S. on March 11, 1918 at Ft. Riley, Kansas, when an Army private reported for sick call complaining of a fever, sore throat and headache. Within a few hours, the number of soldiers reporting in with similar symptoms rose to over 100. Within a week, more than 500 were down with the flu.
Over the course of the summer, the Spanish Flu spread from city to city, and around the world. Ironically, Spanish Flu's spread in the United States was, to a degree; facilitated by bond rallies which brought together large numbers of people in tightly packed crowds. As public health officials eventually came to recognize the dangers, many of these events were cancelled. But for hundreds of thousands, who were infected, this action came too late.
It was not just the U.S. that was effected. Troop ships going to Europe often served as incubators for infection. Indeed, on World War I battlefields, commanders sometimes lost as many troops to the flu as to enemy fire.
In the peak month of Spanish Flu infections, October 1918, fully 195,000 Americans would fall victim to the disease.
 By
the time a vaccine was developed in November of 1918, the disease had largely
run its course, so it was too late to help most of the flu's victims. It remains
the deadliest epidemic ever to reach U.S. shores. It also holds a number of
critical lessons for the dangers that face the developed world today.
By
the time a vaccine was developed in November of 1918, the disease had largely
run its course, so it was too late to help most of the flu's victims. It remains
the deadliest epidemic ever to reach U.S. shores. It also holds a number of
critical lessons for the dangers that face the developed world today.
Perhaps the most important lesson is how rapidly a virulent infectious disease can spread if steps are not taken early on to stem the tide. Had the first cases been quarantined and large public gatherings restricted when the Spanish Flu first appeared, its death toll might have been significantly reduced.
A second important lesson is the need to maintain communication about matters of public health.
As the Spanish Flu spread across the U.S. many believed it the product of a German plot. Other fanciful notions concerning the source of the infection ranged from cat hair to coal dust. Folk remedies and cures also were widely touted. Onions, garlic and goose grease all had their advocates. Unfortunately, while there is little evidence that such curatives actually did any good, they did serve to divert attention from steps, which might help stem the epidemic. Alarmed at the confusion, Surgeon General Rupert Blue argued that bans on public assemblies might be one of the most effective tools to stop the spread of infection. He also warned against the folk remedies and patent medicines being widely touted saying that:
"The Health Service urges the public to remember that there is as yet no specific cure for influenza and that many of the alleged cures and remedies now being recommended by neighbors, nostrum vendors and others do more harm than good."
The lesson of 1918 is clear. Early identification of potential epidemics is vitally important. If the first victims of the Spanish Flu had been quarantined, its spread might have been checked. So too is the need to move quickly to take whatever steps are available to step the tide. Unfortunately, it appears that the lesson of 1918 is one the world has failed to learn. There is an epidemic on the horizon, but few seem willing to recognize its existence.
TB: THE GLOBAL EPIDEMIC
By the late 1970s, it was widely believed that by the end of the century, tuberculosis might be totally eradicated. This appeared reasonable as TB rates steadily declined following World War II. In the middle 1980s, however, it became increasingly evident that there was little basis for such optimism. In the industrialized West, TB rates stabilized, and in the developing world they began to rise. Today, tuberculosis has reached epidemic proportions in some lesser-developed countries.
The World Health Organization reports that tuberculosis kills between 2 million and 3 million people each year. Some 8 million become sick from the disease. To put these figures in perspective, TB kills more people each year than AIDS, malaria and tropical diseases combined. Indeed, it is the leading cause of death in the developing world.
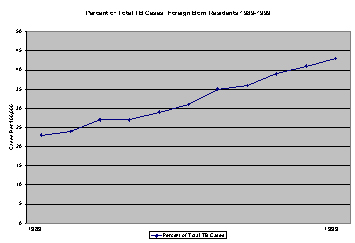 While
significant progress has been made in eliminating TB in the United States, the
job is far from complete. In 1998, the latest year for which data is available,
18 states reported at least 100 cases of TB, and every state reported at least
one case. California, Florida, Illinois, New York and Texas had the highest
number of reported cases, representing 54 percent of the total. The prevalence
of TB cases in New York and California is attributed in part to their substantial
foreign-born populations. The proportion of TB cases represented by the foreign-born
has steadily increased in recent years.
While
significant progress has been made in eliminating TB in the United States, the
job is far from complete. In 1998, the latest year for which data is available,
18 states reported at least 100 cases of TB, and every state reported at least
one case. California, Florida, Illinois, New York and Texas had the highest
number of reported cases, representing 54 percent of the total. The prevalence
of TB cases in New York and California is attributed in part to their substantial
foreign-born populations. The proportion of TB cases represented by the foreign-born
has steadily increased in recent years.
More disturbing were reports of drug resistance among TB isolates (MDR-TB). Overall, 8.1 percent of all cases (1086) showed resistance to at least isoniazid. Roughly 150 cases (1.1 percent) of isolates resistant to both isoniazid and rifampin, i.e. Multi-Drug Resistant Tuberculosis, were reported. Almost half of these cases were reported by New York and California. Among foreign-born residents, the proportion of MDR-TB cases increases 31 percent. Indeed, it is the advent of MDR-TB that holds the seeds of worldwide disaster.
THE ROOT OF THE PROBLEM
Like other drug-resistant strains of bacteria, the advent of Multi-Drug Resistant Tuberculosis is most likely a consequence of the misuse of antibiotics, particularly in the developing world.
Typically, tuberculosis is treated with a combination of drugs that have two essential properties: antibacterial activity and the ability to inhibit the development of resistance. The Centers for Disease Control and Prevention protocol for treatment of TB in adults calls for the use of a combination of isoniazid, rifampin, pyrazinamide and either ethambutol or streptomycin. The treatment is generally continued for a period of roughly six months in routine cases. If the disease progression is severe, however, the treatment may take as long as one year. Where the conventional treatment is successful, improvement will be observed in the patient within a month.
Patient compliance, however, has been a major problem in treating conventional tuberculosis. For many patients, especially in developing countries, the importance of taking all of their medication on a regular schedule is simply not well understood. Also, the cost of medications can prove problematical in poverty-stricken nations. Whatever the cause, poor patient compliance has had a devastating consequence: the advent of Drug Resistant and Multi-Drug Resistant Tuberculosis.
MDR-TB: THE SEEDS OF AN EPIDEMIC
The World Health Organization (WHO) estimates that more than 50 million people are currently infected with Drug Resistant TB. In a March 2000 report, the WHO documenting the prevalence of MDR-TB in some 38 "Hot Spots" around the globe. In several, specifically Estonia, Latvia, China, Iran and Russia, the rates of infection have reached alarming proportions. In Estonia, for example, 18 percent of all TB cases were of the Multi-Drug Resistant strain - up from 14 percent in 1997. But, the phenomenon is not limited to regions outside the developed world.
The Canadian Bureau of AIDS, STD and TB reports that all but two provinces in Canada have experienced cases of Drug Resistant TB. A 1998 study by the Bureau found that 11.8 percent of all TB cases in Canada evidenced some drug resistance, and 1.2 percent were MDR-TB.
 One
of the "Hot Spots" causing the greatest concern is the Russian prison system.
According to a survey of Russian prisons by Medecins Sans Frontiers (Doctors
Without Borders) more than 10 percent of all inmates - roughly 110,000 individuals
- are infected with TB. Of these, roughly 30 percent are infected with MDR-TB.
With some 300,000 prisoners released annually, this means that around 10,000
individuals infected with MDR-TB will enter the civilian population each year.
Since every individual infected with MDR-TB could infect from 10 to 14 people
over the course of a year, by 2010, Russian could have as many as one million
of its citizens infected with MDR-TB. A 1999 report by the Public Health Research
Institute echoes the concern over the situation in Russian prisons stating:
One
of the "Hot Spots" causing the greatest concern is the Russian prison system.
According to a survey of Russian prisons by Medecins Sans Frontiers (Doctors
Without Borders) more than 10 percent of all inmates - roughly 110,000 individuals
- are infected with TB. Of these, roughly 30 percent are infected with MDR-TB.
With some 300,000 prisoners released annually, this means that around 10,000
individuals infected with MDR-TB will enter the civilian population each year.
Since every individual infected with MDR-TB could infect from 10 to 14 people
over the course of a year, by 2010, Russian could have as many as one million
of its citizens infected with MDR-TB. A 1999 report by the Public Health Research
Institute echoes the concern over the situation in Russian prisons stating:
"The tuberculosis epidemic in Russia, particularly Russian prisons has reached alarming proportions. The prison system acts as an epidemiological pump, releasing into society tens of thousands of active TB cases and hundreds of thousands of infected individuals each year. The high rate of multi-drug resistant tuberculosis among them is especially threatening."
The report warned that "transnational cases"; infections contracted in one country and then transported to another will become increasingly common. This notion is supported by the fact that the proportion of reported TB cases accounted for by foreign-born residents in industrialized nations such as the United States and Canada have been rising for several years.
The question, however, is what to do to prevent the problem from becoming a global pandemic. Fortunately, there is an answer.
MEETING THE CHALLENGE
Initially it was believed that the global TB epidemic could be successfully combated with a treatment regime termed "Directly Observed Treatment- Short Course", or "DOTS." Under the DOTS regime, trained health care workers or volunteers directly monitor patients to ensure that they take their medication during the first two months of treatment. This is followed by one of two options. Either the patient continues Directly Observed Treatment for a period of four months, or self-medicates without supervision for a period of six months.
| TUBERCULOSIS BURDEN BY REGION 1997 | ||
| REGION | NEW CASES | DEATHS |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Where the DOTS regime is properly implemented, it has met with considerable success. The trouble is that compliance with the DOTS protocols are not always followed. As a consequence, in some cases it actually can do more harm than good. The failure to complete treatment regimes is the single most important cause of the rise of Drug-Resistant and Multi-Drug Resistant strains of TB. Two studies published in the March 13, 2000 edition of the Archives of Internal Medicine underscore this point.
One study was conducted by Dr. Jordan W. Tappero of the Centers for Disease Control and Prevention it Atlanta. It examined 460 Mexican TB patients for signs of Drug-Resistant and Multi-Drug Resistant strains of TB. The study found that 51 percent of the patients who were being treated for TB a second time showed resistance to one or more of the "first line" TB drugs used in Mexico. Some 22 percent of these patients exhibited Multi-Drug Resistance. Another study of 228 Mexican TB patients conducted by Dr. Maria de Lourdes Garcia-Garcia of Avenida Universidad in Cuernavaca, Mexico found some degree of drug resistance in 28 percent of the patients and multi-drug resistance in 11 percent.
The results of these two studies are not unique. But they point to the inadequacy of current programs to stem the tide of MDR-TB. Clearly a more effective approach is required. While the approach should continue the use of DOTS where appropriate, it must also include the administration of the advanced antibiotics proven effective against MDR-TB. This strategy has been termed "DOTS-Plus."
SELECTING THE ADVANCED ANTIBIOTICS
Multi-Drug Resistant Tuberculosis presents a daunting treatment challenge. Patients are often debilitated, having already undergone an unsuccessful conventional treatment regime. In addition the treatment regime for MDR-TB can take much longer - up to two years - than conventional therapy. Therefore, it is essential that the drugs selected have significant bactericidal properties, and that they can be administered at dose levels patients can tolerate for extended periods of time. In addition, the advanced antibiotics should have significant inhibitory properties to help prevent the development of resistant strains of bacteria.
The family of drugs known as fluroquinolones best meet these criteria. In terms of potential treatments for MDR-TB, the most promising of the fluroquinolones are sparfloxacin, levofloxacin, ofloxacin, ciprofloxacin and pefloxacin. While all of these drugs are of some value in the treatment of MDR-TB, there is considerable variation in their effectiveness.
For example one study conducted by LaLande et al and published in the March, 1993 Journal of Anti-Microbial Agents and Chemotherapy noted that sparfloxacin was
"Six to eightfold more active than OLO (ofloxacin) in preventing mortality and gross lesions in mice infected with M. tuberculosis."
More recently, a study by Guillemin, et al published in the August 1998 issue of the Journal of Anti-Microbial Agents and Chemotherapy found that sparfloxacin was the most active of the quinolones followed by levofloxacin and ciprofloxacin. Hoffner, et al came to a similar conclusion in their 1997 article published in the British Journal of Antimicrobial Chemotherapy.
Given the extensive research over more than a decade indicating that sparfloxacin is the most effective fluroquinolone for the treatment of MDR-TB it would appear that it should serve as the cornerstone for the "DOTS-Plus" therapy in combination with one or more of the other drugs in that family.
Determining what drugs to use, though, is only the first step in implementing the "DOTS-Plus" therapy based strategy. What must be decided as well is where how and when the therapy will be employed. Here, the most productive approach would be to target MDR-TB "Hot Spots." Among the most important of these is the Russian prison system.
TARGETING "DOTS-PLUS"
There are a number of reasons why the Russian prison system is such an important target for the "DOTS-Plus" approach. First of all, it has one of the highest proportions of MDR-TB in the world. Second, because at least 10,000 active MDR-TB cases are released from Russia's prison into the general population annually, the potential for the disease to spread is enormous.
Additionally, the increasing commerce between Russia and the United States makes the potential for transnational infections extremely high. But the most important factor may be the potential for an epidemic of MDR-TB to destabilize Russian society.
Russia already suffers from a host of social ills. Its economy has teetered on the verge of collapse since the demise of the Soviet Empire. Ethnic and political rivalries have shattered national cohesion. Russia's military is demoralized, with many of its members living in abject poverty. Anti-western sentiment is on the rise. Given all of these factors, just as the Black Death gave rise to social unrest in the 14th century, an MDR-TB epidemic could have similar consequences in the already volatile Russian social fabric. But, this time there is more at stake than the potential for peasant revolts or the authority of the Church.
Russia still possesses a massive nuclear arsenal and substantial conventional arms. There is no question that in the wrong hands these armaments could pose a threat to world peace. A destabilized Russian society faced with an MDR-TB epidemic could provide an opportunity for anti-western elements in that nation to wrest control from more progressive forces. Therefore it is in the national interest of the United States to do what it can to help prevent such an eventuality. Helping Russia curb the alarming rise in tuberculosis through a "DOTS-Plus" program is one way to accomplish this goal. It would be a small price to pay to ensure a stable Russian society.